Sommaire
- L'humanitaire au cœur de l'entreprise : enjeux & opportunités, retours d'expérience !
- Congrès International A3P 2018 : restitution des messages clés de la table ronde sur la révision de l'Annexe 1.
- Impact of Annex 1 revision on new vial filling line at Sanofi Pasteur Marcy-l'Étoile.
- Quantitative evaluation of microorganisms recovery from surfaces using contact plates.
- Investigation by molecular method of potentially non-compliant aseptic process simulation-media fill test (APS-MFT) and sterility test.
- Aseptic Processing Overview.
- L'industrie pharmaceutique : renforcer la culture de la qualité.
- Sauvegarde, réplication et archivage... Quelles mesures prendre pour préserver l'intégrité de vos données ?
All facilities and equipment used for the manufacture of sterile injectable products are coming under increasing scrutiny by Health Authorities. The expectations of Health Authorities are increasing. Interestingly, it is difficult to determine if Health Authorities have raised the bar as a result of technological advancements. Or, have Health Authorities adjusted standards for compliance upward as an incentive for improved manufacturing tools?
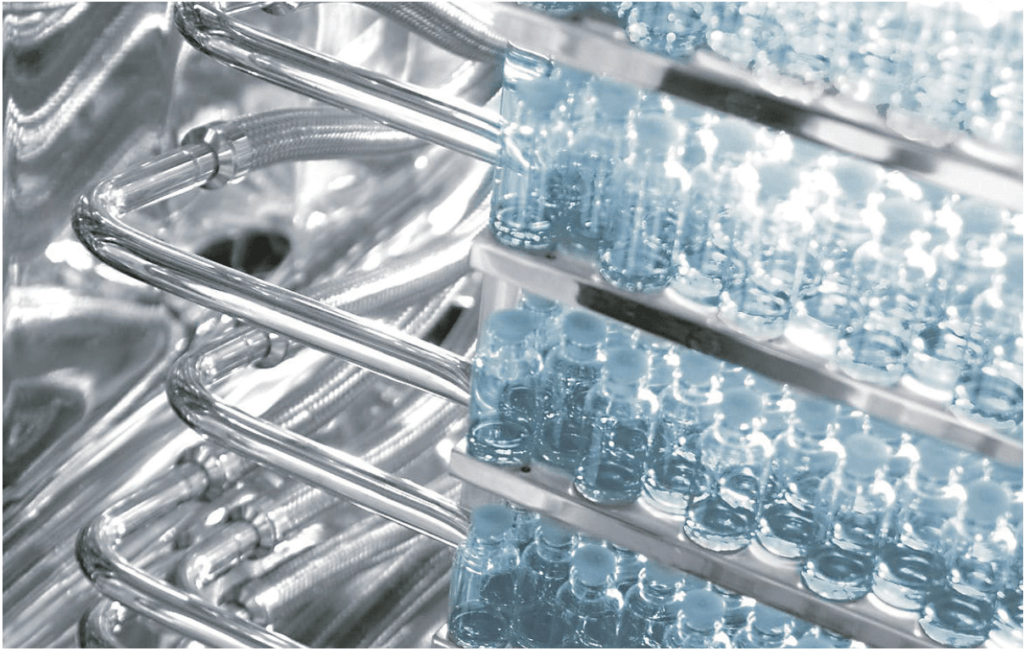
Regardless, regulations and technologies are evolving together and, therefore, they are factors that must be considered when investing in new or renovated sterile manufacturing facilities. These factors are true for all sterile injectables, but the emphasis for this article will be on biologicals and vaccines that are dependent on contemporary microbiological methods for each step of the manufacturing process. This article discusses elements of a microbial control strategy in support of manufacture of sterile injectable products and aspects of control strategies to prevent contamination.
1. Historical Context
There are several pharmaceutical or biological products that must be sterile. These include a range of products that are introduced into patients through routes of administration that include intra-muscular, intra cutaneous, or intravenous. Medications for ophthalmic use must also be sterile. The rationale is that products designed for injection must not introduce contaminating microorganisms. This is because these prophylactic products are injected into healthy individuals and adverse events from contamination are unacceptable. Likewise, therapeutic products must not exacerbate the condition for which these products are intended to treat. Only those products containing attenuated microorganisms as an antigen or as a therapeutic vector can circumvent the requirement for sterility. In this instance, if the attenuated microorganism were not present, the product must be sterile. Regardless of whether the product is prophylactic (e.g., vaccines) or therapeutic (e.g., antibiotics, biopharmaceuticals etc.), public acceptance and trust is fully dependent on an injectable medications safety profile.
The fundamental process design for sterile units of operation can be roughly divided into two different approaches. Each includes a transfer of a solution from a delivery vessel to a receiving vessel. One approach for product transfer is a design to transform the product. The equipment through which the product is processed in the transfer changes one or more attribute. Noteworthy examples for this approach include:
- Sterilization by filtration (non-sterile to sterile),
- Mixing heterogeneous components (e.g., pooling or formulation) to homogeneity
- Combining an “active” ingredient (e.g., toxin, microbe, etc.) with an inactivating agent to form an inactive ingredient.
A non-transformational process for sterile solutions (or powders) could be described as a manufacturing step that moves a substance from one sterile container to another. There are no changes to product attributes associated with this transfer. In fact, there are many instances in which a great deal of emphasis is placed on transferring the product without change. A few examples for this process include:
- Dispensing into sample vessels for analytical testing
- Dispensing to other vessels for shipment, storage, or further manufacture.
- Dispensing to final containers for administration to patients.
In each of the examples above, the requirement for aseptic processing evolves validations to substantiate that equipment is sterile and the system is integral and impervious to ingress of contaminating microorganisms. While it may be slightly oversimplified, aseptic processing of sterile materials could be described as transfer of solutions with or without a transformational event without introduction of contaminants.
Evolution of facilities and equipment for sterile manufacturing has evolved since the 1920s when standards for injectables were established. From the time of mass production of injectables until the 1980s, the state of the art for equipment used to manufacture injectables was marginally adequate for preventing contamination. Some products (e.g., vaccines) that were developed in the 1940 are manufactured today by procedures that remain surprisingly unchanged. It was therefore common to add a preservative as an added measure of sterility assurance. Beginning in the 1920s, vaccines, immunoglobulin preparations, skin test antigens, antivenins, ophthalmic and nasal products, and tattoo inks were formulated to contain one such preservative, thimerosal, an organomercurial compound effective in killing contaminating microorganisms(3). During these times, it was common, though not widely publicized, to delay execution of a sterility test for a short period of time so that any residual microorganisms could be reduced by the effects of the preservative. It was during the 1980 that the evolution of today’s sterile manufacturing methods began.
2. Evolution
The evolution of fill/finish processing began in the early in the 20th Century and during the World War II became widespread when injectable medications became needed for lifesaving or serious injuries.
Aseptic process during these early days was performed using Bunsen burners to flame sterilize connections. Process vessels were generally constructed from glass. Transfers between vessels, as well as sample collections, were in open clean backgrounds and highly subject to contamination. Cotton plugs or rubber stoppers were used to protect glass vessels from additional contamination. It was during the 1930s and following decades that membrane filters became available and were adopted by pharmaceutical manufacturing. And it was in 1939 that one of the first sterile transfer chambers was introduced. It may surprise the reader that some of these manufacturing methods remain in use today.
Over the decades following World War II, sterile manufacturing facilities and equipment were improved. The state of the art for connections and vessels were enhanced following introduction of equipment constructed from stainless steel. Facility improvements included introduction of HEPA filters for clean room air essentially free from particulate matter. These technologies predominated the industry from the 1940s until the late 1970s without a great deal of regulatory oversight until governments’ worldwide published guidance for Good Manufacturing Practices (GMP).
Since the introduction of injectable products, it was widely recognized that microbial contamination was to be avoided. Injection of contaminated drug product was well known to lead to serious adverse events including death. Lack of sterility assurance is a leading contributor to safety alerts and product recalls. Therefore, it was/is an imperative for injectable products to be sterile. The definition of sterility of a material (generally solutions) is one that is absolutely free from living microorganisms. For vaccines containing attenuated/living antigens, this meant it was imperative for this class of product to be pure and devoid of adventitious agents or other contaminating materials.
3. Advancement
Sterility and purity are related terms. Sterility and purity share the need to be absent of contaminating bacteria, fungi or other extraneous agents. However, a pure seed culture cannot be claimed to be sterile for the obvious reasons that seeds are, by definition, not sterile. All seed cultures (Master seeds, working seed stocks, and working seeds) must be manufactured under controlled conditions. Because preservation and expansion of the antigen or therapeutic protein must be achieved with a living microorganism, these steps cannot be sterile. For this reason, purity controls are necessary for seed manufacture at every step up to and including inoculation of starter cultures for and scale-up to fermenters or bioreactors. Purity controls confirm adventitious agents (e.g., bacterial and fungal agents, cultivatable and non-cultivatable mycoplasmas, mycobacteria and viruses) are not present in the Master Seed nor are they reintroduced during manufacture of working seeds. Validations replicating seed manufacturing are the purity controls needed to establish that seed manufacturing steps are adequate for preventing contamination. The validation most widely regarded for validating integrity of seed manufacturing processes is an Aseptic Process Simulation/Media Fill Test. As with other media challenges, it is critical to replicate the process along with good Aseptic Technique and cGMP practices. These controls for purity are an additional assurance that the final material harvested from bioreactors or fermenters are completely free of any adventitious agent. It is a Health Authority expectation that fermentations and/or bioreactor cultures are be free from other living or infectious material.
There are several examples during upstream manufacture of a biological drug substance in which is it impractical to utilized closed manufacturing process equipment. That is, state of the art equipment for some application cannot be operated as closed and contained and be able to achieve process requirements(1). Open processing is not capable of achieving aseptic conditions and, therefore, does not prevent movement of microorganisms (bioburden) from the environment into product stream. Thus, it is impractical, if not impossible, to perform all of the steps associated Drug Substance manufacture without allowing for some, albeit small, number of contaminants. Bioburden controls provide for monitoring and management of open processing steps. Notwithstanding equipment limitations, rigorous monitoring of bioburden levels and use of process equipment to control bioburden at the lowest attainable level are necessities for the establishment of bioburden Alert and Action Limits. The goal for bioburden control measures should be the lowest level of bioburden that is achievable by capability of the process.
A question that many firms wrestle with today is when to claim sterility for an intermediate or excipient that will be stored for an undetermined period of time. There is very little regulatory or industrial guidance, and certainly no consensus, on which solutions should be sterilized and claimed sterile. The microbiological consideration is that any solution having a carbon source, trace minerals, and an absence of bactericidal/bacteriostatic agents is at risk for proliferation of contaminants. Most injectable products released to the market are assembled from components that once were non-sterile. The microbial quality of these products is ensured because the manufacturers are required to perform initial and periodic revalidation of the sterilization steps for products and processes equipment. To accomplish this, an imperative is to know the microbial content of materials sterilized prior to the sterilization step to evaluate the Sterility Assurance Level (SAL) of materials sterilized. For this evaluation, compendial tests for microbial enumeration are used and an essential function of testing laboratories.
For intermediates not claimed sterile, contamination control practices are necessary prior to steps in the end-to-end manufacturing process in which the process output is sterile. The risk that should be in the forefront of process design is to contain non-sterile solutions in a manner that prevents contamination of microorganisms that could replicate. In fact, a solid contamination control strategy should be put into place for each unit of operation prior to and following the sterile boundary. It is prudent to practice good Aseptic Technique and contamination control throughout manufacture of sterile injectables.
With the exception of products that are terminally sterilized or chemically inactivated, sterile injectable products will be sterilized by filtration(5). For this reason, new installations and upgrades for the manufacture of heat labile biologicals should be constructed using modern approaches to close and contain each unit of operation. A key decision for process design is the unit of operation that defines the sterile boundary. While there may be a filter sterilizing step for two or more units of operation, the first step to be claimed sterile should be considered to be the sterile boundary. Following the sterile boundary, the process design should be closed for units of operation downstream from the first sterilizing grade filter. The evolving technologies for designs mating stainless steel and single use technologies renders manufacture of Drug Substance and Formulated Drug Product affordable and feasible for closed systems highly robust for prevention of contamination.
Aseptic processing requires practices that safeguard processing of sterile fluids known as aseptic techniques. Aseptic techniques include a broad range of actions, behaviors, and equipment to prevent contamination. These tools become an imperative for a few biological products that are not sterilized at any unit of operation in the end-to-end manufacturing process. There are also a number of intermediates having a composition that cannot be sterilized by filtration downstream of a given processing step. In instances such as these, the biologic substance or unfilterable intermediate are comprised of materials too large to pass through a microporous filtration membrane. In the first instance, the material must be sterile beginning with the first manufacturing step, seed inoculation, and remain sterile at each subsequent step. In both instances, unfilterable materials must be sterile and process by strict aseptic technique to prevent contamination. This means that every product contact surface must be sterile before becoming exposed to sterile biological materials.
4. Avoiding Contamination
What are the consequences should the solution become contaminated? Biological manufacturing is a complex enterprise because the units of operation employed to produce a biotherapeutic or vaccine antigen must use living cells(2). As stated earlier, the media used for expansion of the biologic of interest must contain a carbon source and other essential ingredients for microbial proliferation. While there can be substantial purification of the biological material of interest, in the end, purified materials remain in a milieu that preserves most of the attributes needed for microbial proliferation. Adventitious agents of greatest concern include bacteria and molds/fungi. In instances in which a biologic is replicated in tissue culture cell, viruses (especially non-cytopathic viruses) should be given serious consideration. This is the case even in instances in which cell substrates are thought to be non-permissive. In the absence of effective barriers, microbial contaminations adversely impact on biologic product manufacture. Contaminants introduce product variability that can lead to potency losses from degradation or to a deleterious modification of product by microbial enzymes. Contaminants can change impurity profiles and increase bacterial endotoxins. In addition, the investigations of microbial contaminations can result in lengthy shutdown periods and delays in manufacturing operations that in turn, may sometimes result in shortages of essential drug products. Strict microbial production controls are essential to ensure the manufacture of a drug product with consistent quality. In this regard, a well designed risk assessment may be of great value. The purpose of such a risk assessment should not be, as is too often the case, to justify a poor or weak practice. Rather, a risk assessment for this topic can be an invaluable tool in the identification and correction of potential failure modes that can be fortified with closed systems.
What is the value of a sterility test? A sterility test is not a precise and comprehensive evaluation of the status of the test object. Recall it was stated earlier that a sterile material is absolutely free from living microorganisms. For a test to confirm a batch to be sterile, one would need to test 100% of the batch. In the case of product in final filled containers, such a test is unachievable. For that reason, a sample from filled batches is tested. Pflug published a statistical analysis that describes the probability of a detection of a contaminant in batch of final containers(4). The likelihood for detection is high only for those batches in which there exists major contamination. For example, if 5 (0.0005%) final containers in a batch of 100,000 were contaminated and the number of test articles was 50, then the probability of detection would be 1 in 400. In other words, the sterility test would require 400 replicates in order to detect a single contaminated unit. By contrast, if 10,000 (10%) containers in a batch of 100,000 were contaminated and the number of test articles was 50, then probability is almost certain the contaminants would be detected with a single test(6-7).
Regulatory authorities are in general agreement that a sterility test indicates that within the conditions for which the test was performed, no microorganisms were detected. So again, what then is the value of a sterility test? Perhaps the commonly recognized value of a sterility test is that it offers some reassurance that there is not a level of contamination that was detected. Elements of this reassurance are built into the stringent conditions in which the test is conducted. By contrast, in circumstances in which microorganisms were detected, the test provides ample information for rejecting a batch. Furthermore, identification of the contaminant is generally quite useful in root cause analysis and corrective action. Thus, the value of the sterility test in defining, with high confidence, that a batch is grossly contaminated. So if sterility tests only detect “gross failures”, how then is sterility established? Quite simply, sterility is established through the assurances provided in designs for facilities and process equipment, validation of the sterility of product contact surfaces in process equipment, training/proficiency of operators, and contamination control measures at every step of the manufacturing process. The validation that essential to establish sustainability of sterile manufacturing operations is the Aseptic Process Simulation/Media Fill Test. It is only this validation that challenges all of the elements that are needed to deliver a sterile injectable product(9-10).
Sterility is an imperative to that contributes to public trust that injectable products are safe from transferring an infectious disease. It is for this reason that Health Authorities place great emphasis on manufacturing practices. The evolution of process equipment for the key steps in sterile manufacturing allows for a very high level of sterility assurance for sterilization and storage of biologics.
Sterility is an absolute that cannot be affirmed without testing 100 percent of a solution or final filled batch. Testing for sterility is only a product release function that provides that the batch is not grossly contaminated. Health Authorities in the European Union (Annex 1) and the United States (FDA) along with the World Health Organization (WHO) share a common view. It is only through validation of aseptic procedures that sterility can be affirmed.
Sterility involves in-depth understanding of the failure modes for contamination and validations that establish that the process equipment and facilities are robust. A risk analysis to justify a poor practice is a prescription for failure. Rather, use of a risk assessment to identify failure modes followed by remediation is an approach that will sustain acceptable performance.
Partager l’article

Joseph C.FRANTZ – SANOFI
joseph.frantz@sanofi.com
References
(1) J. Agalloco and L. Mestrandrea, ” Moving to Closed Systems for Aseptic Processing,” Pharmaceutical Technology and BioPharm International Vaccine Development and Manufacturing 2017 eBook (November 2017).
(2) Stanley Plotkin,a James M. Robinson,b, Gerard Cunningham,c Robyn Iqbal,d and Shannon Larsenb The complexity and cost of vaccine manufacturing – An overview. Vaccine. 2017 Jul 24; 35(33): 4064–4071
(3) Sharpe, M. A.; Livingston, A. D.; Baskin, D. S. (2012). “Thimerosal-Derived Ethylmercury is a Mitochondrial Toxin in Human Astrocytes: Possible Role of Fenton Chemistry in the Oxidation and Breakage of mtDNA”. Journal of Toxicology. 2012: 1–12.
(4) Validation of Aseptic Filling for Solution Drug Products, PDA Technical Monogram, Number 2, pub. 1981.
(5) Maik W. Jornitz, Peter G. Soelkner, and Theodore H. Meltzer. Sterile Filtration – A Review of the Past and Present Technologies. PDA J Pharm Sci Technol July/August 2002 56:192-195
(6) Myths in Pharmaceutical Manufacturing – Microbiological Myths David Hussong, Ph.D., Valsource, LLC 10th Annual PDA Global Conference on Pharmaceutical Microbiology Monday October 19, 2015
(7) Pflug, in Industrial Sterilization, Proceedings of the International Symposium, 1972
(8) Guidance for Industry (2004) : Sterile Drugs Products Produced by Aseptic Processing-Current Good Manufacturing Practice
(9) Volume 4 EU Guidelines to Good Manufacturing Practice Medicinal Products for Human and Veterinary Use Annex 1 Manufacture of Sterile Medicinal Products (corrected version)
(10) Annex 6 WHO good manufacturing practices for sterile pharmaceutical products





