Sommaire
- La restriction des PFAS dans l’industrie : enjeux réglementaires et impacts sur l’industrie pharmaceutique
- La technologie Blow-Fill-Seal dans l’industrie pharmaceutique : performance, applications et durabilité
- Key Allies in Preventing Contaminants and Impurities in Bioproduction
- Choosing the right vial: packaging sterile drug products with foresight
- Combination Products in the United States and European Union: Differences and proposed strategy to prepare common CTD Quality Module 3
- Blood plasma processing. When every drop counts
- L’analyse de la normalité en Continued Process Verification
- Qualification of impurities
- Pharma 2052
Choosing the right vial: packaging sterile drug products with foresight
Effective drug product development demands meticulous container selection. This choice is significant, impacting a drug’s stability, safety, efficacy, commercial viability, and patient acceptance. For biologics, frequently at the forefront of therapeutic innovation, injectable administration is often necessary due to inherent instability and susceptibility to degradation within the gastrointestinal tract. These complex molecular structures respond sensitively to environmental factors, including temperature, light, and packaging material interaction. Such formulations necessitate rigorous sterile manufacturing and filling processes to prevent microbial contamination.
The pharmaceutical packaging landscape constantly evolves, offering a growing array of options beyond traditional glass vials, each with distinct advantages. Selecting the optimal container early in a biologic’s develop- ment, alongside a planned manufactu- ring strategy, is crucial. This foresight helps circumvent costly delays, reformu- lations, and regulatory hurdles.
The final form factor: navigating injectable choices
Selecting a drug’s final fill form is a complex, multifaceted decision. It is influenced by interconnected factors:
– The specific biologic modality (e.g., monoclonal antibody, gene therapy, vaccine),
– The intended route of administration (intravenous, subcutaneous, intramuscular),
– Formulation compatibility with chosen materials,
– End-user or patient preferences.
Given their intrinsic instability, biologics require careful handling throughout the entire manufacturing and packaging pipeline, from upstream processing to final fill, finish, and distribution. Recent advancements in container technologies, particularly pre-filled syringes (PFS) and blow-fill-seal (BFS), fundamentally reshape fill form selection, moving the industry beyond reliance on historical precedents toward innovative, patient-centric solutions.
Beyond glass: the plastic advantage – a deeper analysis
Glass has long dominated pharmaceutical packaging, but alternative materials are joining it on the market. While glass vials remain essential for certain presentations and legacy products, the rise of PFS and BFS technologies signals a shift toward plastic-based solutions. This tran- sition is driven by improved safety, cost-efficiency, design flexibility, and emerging sustainability goals.
Vials, typically borosilicate glass, are established, versatile containers. They are straightforward to fill on aseptic lines and are chemically compatible with many biologic formulations. Useful in early-stage clinical trials due to smaller batch sizes and flexibility, their multi-dose capacity offers convenience but may necessitate preservatives and carries a higher contamination risk with repeated access. Despite their widespread use, glass vials are susceptible to breakage during shipping and handling. Glass delamination – where microscopic glass flakes shed into the drug product – remains a concern for sensitive biologics, potentially affecting product quality and patient safety.
PFS, made from glass or advanced polymers, represents a significant patient care advancement. They enhance dosing accuracy, minimise product waste, and simplify patient self-administration. These attributes suit high-value products requi- ring precise dosing and commercial-scale applications where patient adherence and convenience are key. Their user- friendly design often incorporates safety features to prevent needle-stick injuries, and their inherent precision improves patient outcomes and therapy adherence. Polymer PFS are gaining traction due to their enhanced robustness over glass, reducing breakage risk and particulate generation. The comparison of the rejec- tion rate for breaks/cracks shows that for glass PFS, it is between 0.1 and 0.5% (risk during filling/handling), whereas for polymer PFS, it is close to 0% (very rare due to the strength of the material).
The shift to plastic containers in pharmaceutical packaging is driven by both clinical and logistical advantages. Plastic materials are significantly less prone to breakage than glass, enhancing product safety during transit, storage, and administration, thereby substantially reducing costly product loss from container integrity failures. Plastic’s inherent resilience also reduces handling damage, a notable benefit in clinical settings, emergency situations, and for patient self-administration.
Furthermore, plastic materials inherently minimise particulate contamination. Unlike glass, which can delaminate, pharmaceutical-grade plastics are largely inert and do not exhibit this phenomenon. This is a paramount concern for injectable medicines, as particulates, even if sterile, can trigger adverse reactions or block delivery devices.
Plastic also offers significant design flexibility. Unlike glass moulding’s rigid limitations, plastics can be engineered into diverse shapes, sizes, and functiona- lities. This allows for customisation that improves ergonomic handling, facilitates specific drug delivery mechanisms, or incorporates unique branding elements. Creating integrated components, such as caps or twist-off closures, in a single moulding process can also streamline manufacturing and reduce complexity.
Regarding sustainability, while plastics have an environmental footprint, their lighter weight compared to glass can reduce transportation costs and associated carbon emissions. Reduced breakage also contributes to less waste in the supply chain. Ongoing research into bio-based and recycled pharmaceutical-grade plastics promises to further enhance their environmental credentials.
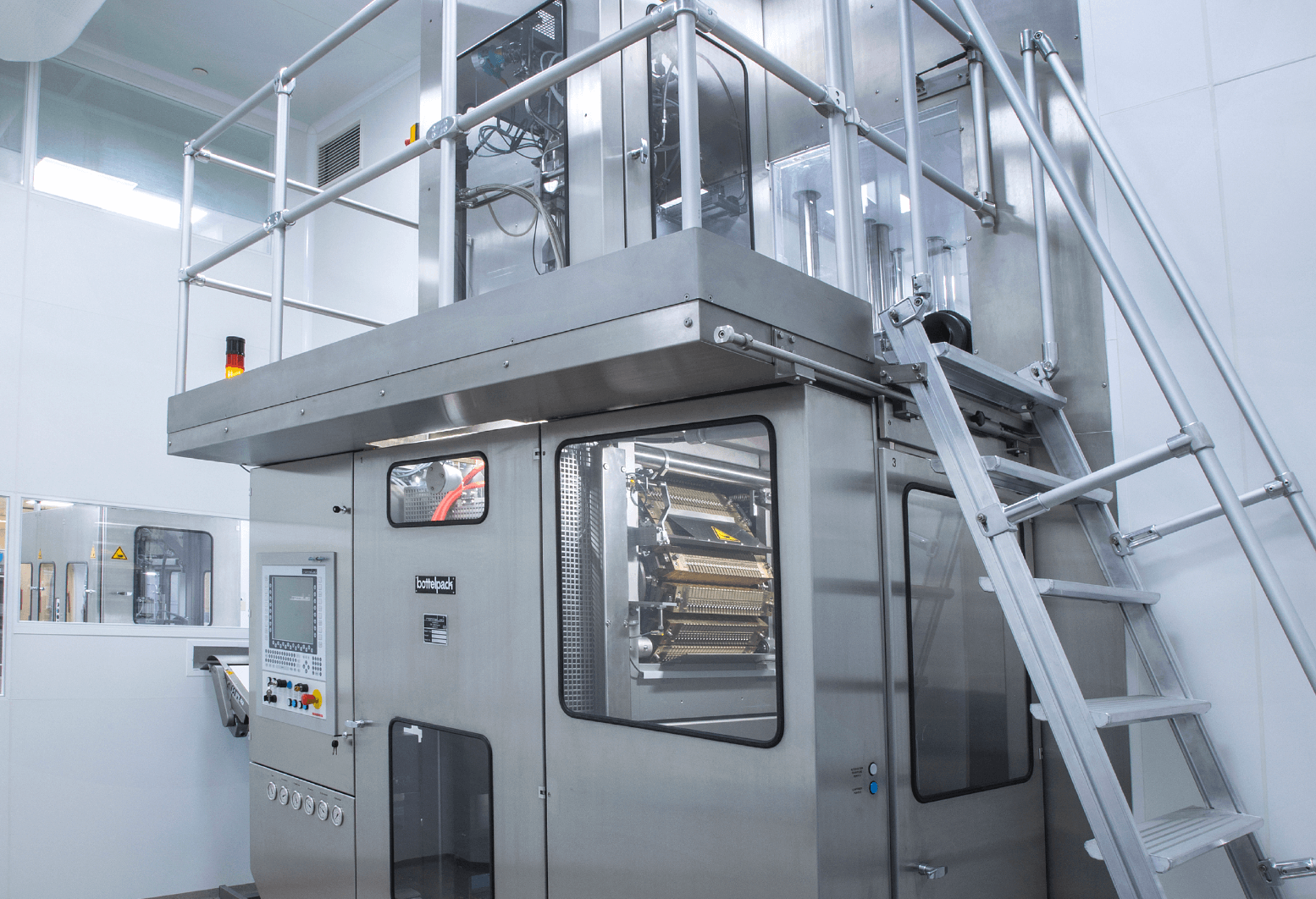
Blow-fill-seal: the benefit of integrated aseptic manufacturing
BFS technology represents an alternative automated fill-finish process where plastic ampoules are simultaneously formed, filled with the drug product, and then sealed within a single, continuous, highly integrated operation. This advanced technology can be utilised for the aseptic filling of diverse products, including ophthalmic solutions, injec- table medications, and, increasingly, vaccines. BFS offers an array of advan- tages, making it an attractive option for sterile drug products, particularly those required in high volumes or with specific safety requirements.
Fully aseptic processing: The intrinsic design of the BFS process ensures an exceptionally low risk of contamina- tion, distinguishing it from conven- tional aseptic filling lines. In traditional methods, pre-formed containers are separately sterilised, then transferred to a sterile filling environment, involving multiple steps and exposures. In contrast, a BFS machine works as a closed system and operates with a molten plastic parison extruded directly into a mould within the machine’s sterile zone. The container is formed by blowing sterile air, immediately filled with the sterile drug product, and then hermetically sealed, all within seconds in a highly controlled, contained, and often ISO Class 5 (Class 100)/Grade A environment. This prevents any human intervention in and near the critical zone, eliminates container pre-sterilisation and subsequent hand- ling, and significantly reduces the potential for microbial ingress. The air used for blowing and product transfer is supplied by 0.22μm hydrophobic filters that have been exposed to steam during an automated sterilisation in place (SIP) sequence. This ensures the air is sterile and provides a robust barrier against contamination. This “Form-Fill-Seal” in one machine significantly simplifies the aseptic chain.
Significantly reduced breakage risk: Plastic containers produced via BFS are inherently less susceptible to breakage compared to glass. In Blow fill Seal, for well-controlled lines in operation, the overall reject rate for leaks is below 0.5%. This resilience is a major advantage across the entire supply
chain, from the manufacturing plant to the point of administration. It directly translates to enhanced product safety during high-speed manufacturing, bulk transportation, storage, and ultimately, during preparation and administration by healthcare professionals or patients. The result is a substantial reduction in costly product loss due to container integrity failures. The inherent flexibility and shatter-resistance of plastic also mean less risk of damage from accidental drops or impacts, a major benefit in busy clinical settings, emergency situations, and for patient self-administration. This robustness also makes BFS ideal for viscous products that might stress glass containers during filling or delivery.
Economic efficiency at scale: BFS technology enables efficient, high-volume filling, leading to a notably lower cost per unit compared to traditional aseptic filling methods. This cost-effectiveness stems from several factors: the raw material (pharmaceutical-grade plastic resin) is often less expensive than glass; the integrated nature of the process reduces the need for multiple machines and associated maintenance; labour costs are lower due to automation; and the elimination of separate container washing, sterilisation, and transfer steps simplifies the overall manufacturing foot- print. This makes BFS particularly bene- ficial for products requiring large-scale, consistent production, such as generic sterile solutions, ophthalmic products, or mass vaccination campaigns where volume and cost-efficiency are critical. High output rates per machine further contribute to economies of scale.
Precision and waste minimisation for single doses: BFS containers are ideally suited for single-dose applications. This provides several benefits: it ensures patients receive the precise amount of medication, eliminating guesswork for patients self-administering or the need for partial withdrawals from multi-dose vials. This precision also significantly minimises the waste of valuable, often costly, medications that can occur with multi-dose vials, where residual drug might be discarded after a single use or due to expiration. The single-dose format also frequently eliminates the need for antimicrobial preservatives in formula- tions, which can be advantageous for patient safety, particularly for ophthalmic solutions or sensitive injectable biologics where excipient minimisation is desired. This also simplifies formulation develop- ment.
Reduced extractables and leachables (E&L) profile: While all container mate- rials have the potential for extractables and leachables, the specific grades of polyethylene (PE) and polypropylene (PP) used in BFS are often chosen for their inertness and low interaction with drug products. These materials are care- fully selected and tested to ensure they do not leach harmful or reactive subs- tances into the formulation. This can be a significant advantage, especially for sensitive biologic formulations highly susceptible to aggregation or degra- dation from trace amounts of certain compounds. The BFS process itself, being closed and rapid, limits the duration of contact between the molten plastic and the drug product, further mitigating E&L concerns compared to longer-term storage in traditional plastic containers. In addition, BFS significantly reduces the number of components in contact with a product, compared with a multidose format – which may feature a separate closure and container. This helps minimise E&L risk.
Tamper-evidence and security: BFS containers inherently offer strong tamper-evident features as embossing or laser engraving on each vial. The hermetic seal formed during the process is difficult to break without visible evidence, providing an immediate indi- cation if the product has been compro- mised. This enhances patient safety and product security in the supply chain.
A real-world application: BFS in vaccine production
The utility and versatility of BFS technology for complex and sensitive biologics were demonstrated in a living attenuated oral vaccine project. This undertaking presented several significant challenges that highlighted BFS strengths: the necessity for stringent product cost management due to anticipated large- scale production, the crucial need to mitigate biological risks associated with handling live attenuated viral material, and the requirement for precise tempe- rature control throughout the entire production cycle.
The experience gained from this project yielded critical learnings for future BFS applications: the importance of utilising the actual product (or a high-fidelity surrogate) for process testing and validation to optimise filling parameters and ensure product integrity; a focus on maximising yield from the valuable bulk drug substance to ensure cost-effectiveness and sufficient supply; and the necessity of meticulously managing temperature fluc- tuations and cold chain integrity, given the temperature sensitivity of the vaccine. For this vaccine project, the inherently aseptic nature of BFS, coupled with its proven reduced breakage risk during high-speed manufacturing and transportation, and its cost-effectiveness for high-volume production, proved instrumental in over- coming these challenges and ensuring a successful outcome for a sensitive and globally significant product. The ability to produce stable, single-dose units further streamlined distribution and administra- tion.
Holistic considerations: beyond the container itself – a comprehensive overview
Beyond the critical choice of the primary container, several other inter- related factors demand close attention throughout biologic development and manufacturing. These elements are intri- cately linked to container selection and overall product quality:
Stability and product longevity: Main- taining the biophysical and chemical stability of biologics is paramount for their safety and efficacy throughout their defined shelf life. Precise temperature control, often in a cold chain (2-8°C) or even ultra-low temperature (e.g., -80°C) environment, is universally crucial for their integrity. The chosen container must be compatible with these storage conditions and protect the delicate biologic from environmental stressors.
The integrity of fill and finish processes: The aseptic fill and finish process requires diligent attention to detail to mitigate risks that can compromise product quality and patient safety. These include:
– Foreign particle contamination: The presence of visible or sub-visible particles (e.g., glass shards, fibres, rubber stoppers, insoluble drug aggregates) can lead to adverse patient reactions or regulatory issues. Strict environmental controls, material selection, and process design mini- mise this. BFS, by its closed and inte- grated nature, significantly reduces environmental particle ingress.
– Silicone concerns: Silicone oil is commonly used as a lubricant for glass pre-filled syringes and stoppers to ensure smooth plunger movement and good container closure integrity. However, silicone can interact with sensitive biologics, potentially causing protein aggregation or particle forma- tion. For some biologics, low-silicone or silicone-free options, including polymer-based syringes or BFS containers, may be preferred or necessary.
– Oxidative stress: Oxygen ingress can lead to oxidation of susceptible amino acid residues within biologic molecules, causing degradation and activity loss. The container’s oxygen barrier properties and headspace oxygen levels during filling are critical. Certain plastic materials used in BFS offer good oxygen barrier properties, and the rapid, closed nature of the process can minimise air exposure. A pouched application around the dose for sensitive products can also be used to further reduce exposure risk.
– Extractables and leachables (E&L): Compounds leaching from the container or closure system into the drug product can impact its stabi- lity, safety, and efficacy. Rigorous E&L studies assess the compatibility between the drug product and all primary packaging components over the product’s shelf life. The selec- tion of medical-grade plastics with well-characterised E&L profiles is paramount for BFS containers.
– Container closure integrity (CCI): Ensuring a robust, hermetic seal is fundamental to maintaining steri- lity and preventing product degra- dation. Comprehensive CCI testing methods (e.g., vacuum decay, helium leak detection, dye ingress) validate the integrity of the sealed container throughout its shelf life. BFS contai- ners, with their fused plastic seal, are inherently designed for excellent CCI.
Regulatory pathways and compliance:
The chosen container and manufactu- ring process must align seamlessly with global regulatory requirements, including those from agencies like the European Medicines Agency (EMA) and the Medi- cines and Healthcare products Regu- latory Agency (MHRA) in the UK. This involves demonstrating product stability and safety, and providing extensive docu- mentation on container materials, manu- facturing processes, and quality control measures. Rigorous testing for container closure integrity, comprehensive stabi- lity studies, and strict compliance with pharmacopoeial standards (e.g., Euro- pean Pharmacopoeia) and Current Good Manufacturing Practices (cGMP) are non-negotiable. The validation of the BFS process isn’t more complex than glass or other PFS technology but requires a complex undertaking, requiring robust studies on aseptic performance, sterilisa- tion parameters, and container integrity.
Supply chain and logistics: Container choice impacts the entire supply chain. Lighter plastic containers can reduce shipping costs and carbon footprint. The robustness of plastic also means less damage in transit, important for products shipped globally.
Looking ahead: navigating future trends with expert partnership
In the evolving landscape of sterile drug product packaging, future trends are driven by patient needs and sustainability. As biologics proliferate, demand for user-friendly, convenient administration methods grows, pushing innovations like PFS and subcutaneous delivery devices. The industry also prioritises greener packaging solutions, reducing material usage and exploring smart technologies for enhanced safety and supply chain inte- grity. BFS (Better Faster and Sustainable) is the perfect technology to combine these matters
Navigating these complexities requires expert collaboration. Partnering with a contract development and manufacturing organisation (CDMO) experienced in biologics is essential. A capable CDMO offers crucial services, including early feasibility studies, robust analytical support, process optimisation, and regu- latory guidance. This strategic collaboration ensures the selection of the right container, leading to compliant products that safely and effectively reach patients, ultimately driving market success.
Partager l’article